Desjardins Insurance
Claims are adjudicated 24 hours a day, 7 days a week, excluding maintenance periods.
If your patient is part of a policy that has migrated to TELUS Health and the claim meets the other prerequisites to be accepted: the Desjardins Insurance response to your claim will be an Explanation of Benefits. If you have made the request, the payment will be issued to the provider or the clinic/organization.
If your patient is part of a policy that has not yet migrated to TELUS Health: the Desjardins Insurance response will be an Acknowledgement. The payment will be made to the insured member.
Desjardins Insurance changed their claim processing system in 2021. All claims are now processed in real time, and payments are being issued to the provider or clinic/organization.
You can void a claim in the portal on the same day. To void a claim the next day or later, please call Desjardins Insurance at 1-800-463-7843 from Monday to Friday, 8 a.m. to 8 p.m.
Contact Desjardins Insurance at 1-800-463-7843 from Monday to Friday, 8:00 a.m. to 8 p.m.
For assistance with the Payment Statements section of the eClaims portal, please contact the TELUS Health Support Centre at 1-866-272-2204.
Monday – Friday: 8:00 a.m. to 12:00 midnight (ET)
Weekends: 9:00 a.m. to 8:00 p.m. (ET)
Public Holidays: 12:00 noon to 8:00 p.m. (ET)
Civic Holidays: 9:00 a.m. to 8:00 p.m. (ET)
Contact TELUS Health at 1-866-240-7492, from Monday to Friday, 8 a.m. to 8 p.m.
A response in real time and payments to providers are now offered for all Desjardins Insurance plan members. The new process offers an improved eClaims experience, including:
A response in real time as soon as the claim is accepted;
Payment issued directly to the provider;
Payment statements available online in the eClaims portal.
Desjardins Insurance processes acknowledgements within 2 business days. Providers receive payment statements twice a month.
Yes. Desjardins Insurance processes all claims in real time and allows the payments to be issued to the provider or clinic/organization for all its policies.
Providers are paid by cheque or direct deposit based on the information provided when registering with TELUS. Payment statements for direct deposit payments are posted on the eClaims portal and payment statements for cheque payments are sent by mail. Payments are issued by TELUS Health, on behalf of Desjardins Insurance, on the night of the 15th and on the last night of each month. The first statement of each month, which you can view on the 16th, includes those claims processed on the previous 15 days. The second statement, which you can view on the first day of the next month (for example, the January 31st statement is available on February 1st), includes those claims processed between the 16th and the last day of the month.
Payments are issued by TELUS Health, on behalf of Desjardins Insurance, on the night of the 15th and on the last night of each month. The first statement of each month, which you can view on the 16th, includes those claims processed on the previous 15 days. The second statement, which you can view on the first day of the next month (for example, the January 31st statement is available on February 1st), includes those claims processed between the 16th and the last day of the month.
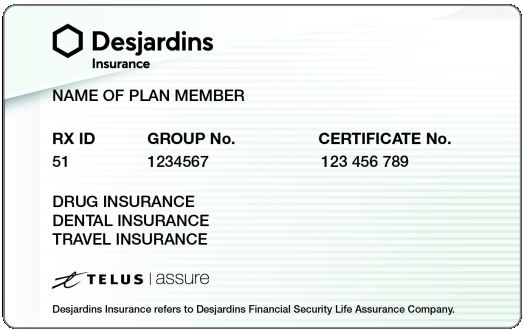
The payer name is TELUS Assure.
Payment statements for clinic/organization administrators are issued per date, regardless of the number of providers. For example, if a clinic has two healthcare providers who both submitted claims to Desjardins Insurance in the last 15 days, both providers are included on the statement. The Details section of the statement identifies the provider type and the name of the patient, as well as the claim ID. You will receive one direct deposit from TELUS Assure for each statement.
Payment statements for providers are issued per location and date. For example, if a healthcare provider works in two different locations, and the provider submitted claims for services rendered in these locations in the last 15 days, you will see two statements—one for each location. For these two statements, you will receive one direct deposit from TELUS Assure.
No, you will not be notified via email if a new payment statement is available. Check the Payment Statements application in the portal on the 16th and last day of each month. The first statement of each month, which you can view on the 16th, includes those claims processed in the previous 15 days. The second statement, which you can view on the first day of the next month (for example, the January 31st statement is available on February 1st), includes those claims processed between the 16th and the last day of the month.
You can print Desjardins payment statements from the Payment Statements application.
No. Only payments are included in the statements.
Coordination of benefits is not available for Desjardins Insurance at this time.
If a second claim is submitted for the same service on the same day, it will be rejected.
The payment statements are offered in the TELUS Health Provider Portal. You will not receive an email indicating that the statement is available, so ensure that you check the portal for statements on the first and 16th of the month. The payer in your bank account will appear as TELUS Assure, as TELUS is providing this additional service and paying providers on behalf of Desjardins Insurance.
The system supports the following healthcare provider roles. Not all of these roles are eligible to submit eClaims in every province.
-
Acupuncturists
-
Athletic therapists
-
Chiropractors
-
Chiropodists
-
Dietitians
-
Guidance counsellors
-
Kinesiologists
-
Massage therapists
-
Naturopathic doctors
-
Occupational therapists
-
Opticians
-
Optometrists
-
Osteopaths
-
Physiotherapists
-
Physiotherapy technologists (Québec only)
-
Podiatrists
-
Psychologists
-
Psychotherapists
-
Sexologists
-
Social workers
-
Speech-language pathologists