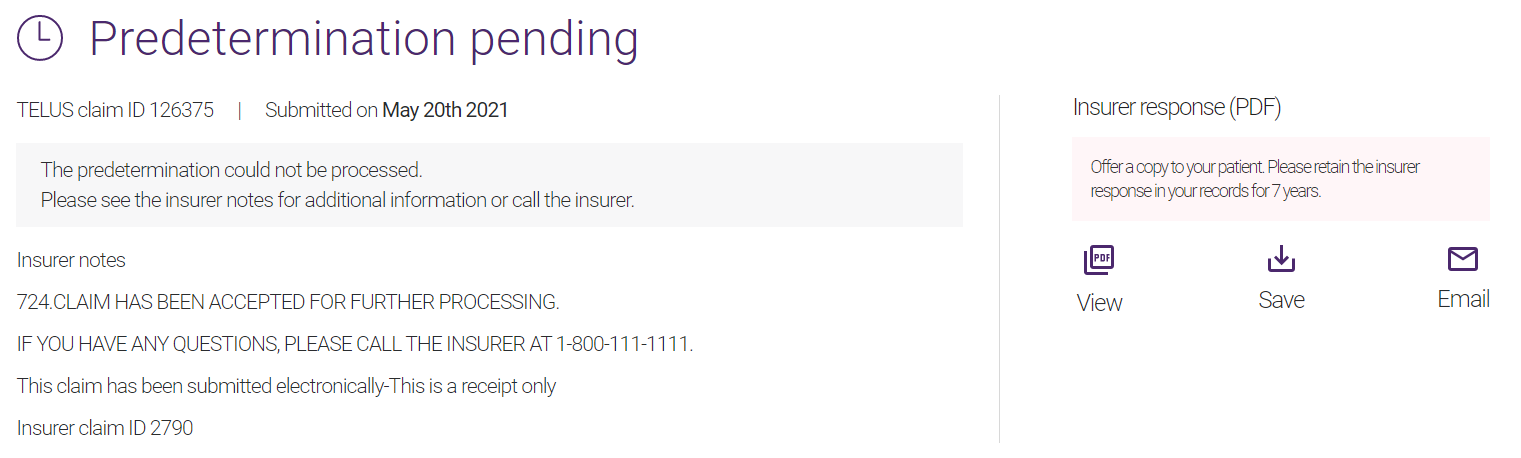
Predetermination pending / acknowledgement
This type of response is generated when the insurance company has successfully received the predetermination request but has not yet accepted it.
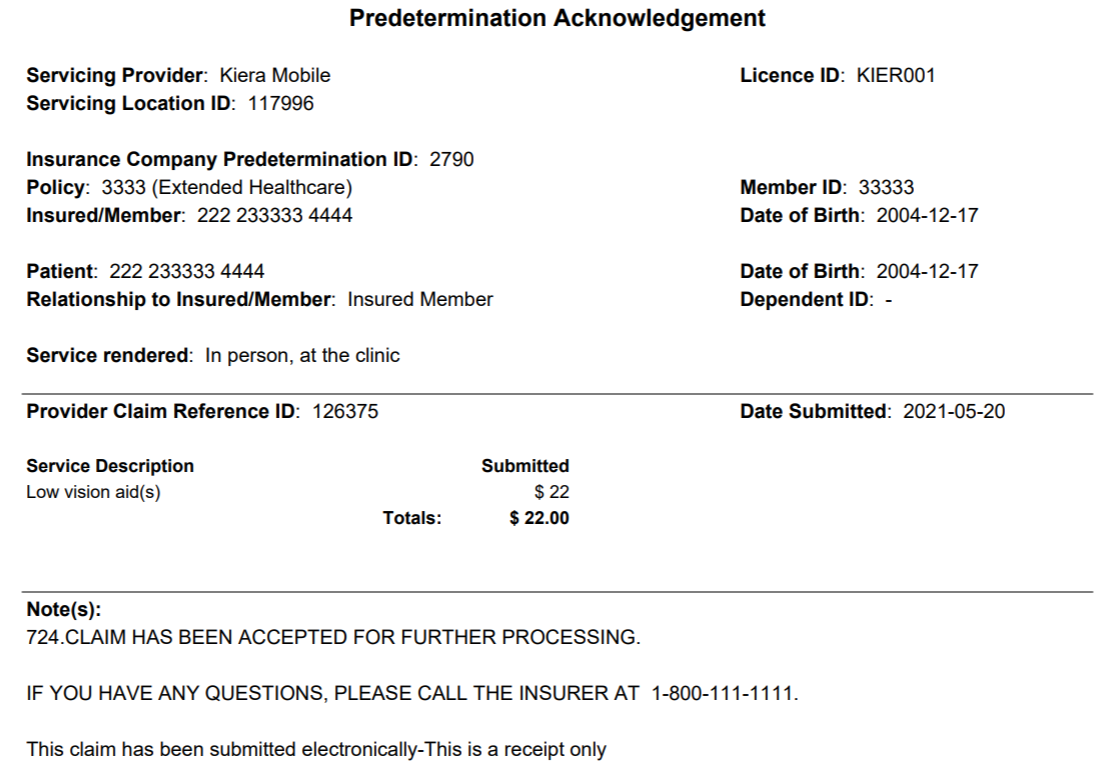
From the Insurer response (PDF) section, you can view or save the Predetermination Explanation of Benefits, or email it to the patient. The Predetermination Explanation of Benefits response provides the estimated amounts, if any, that would be paid by the insurance company if the claim were submitted on that date.