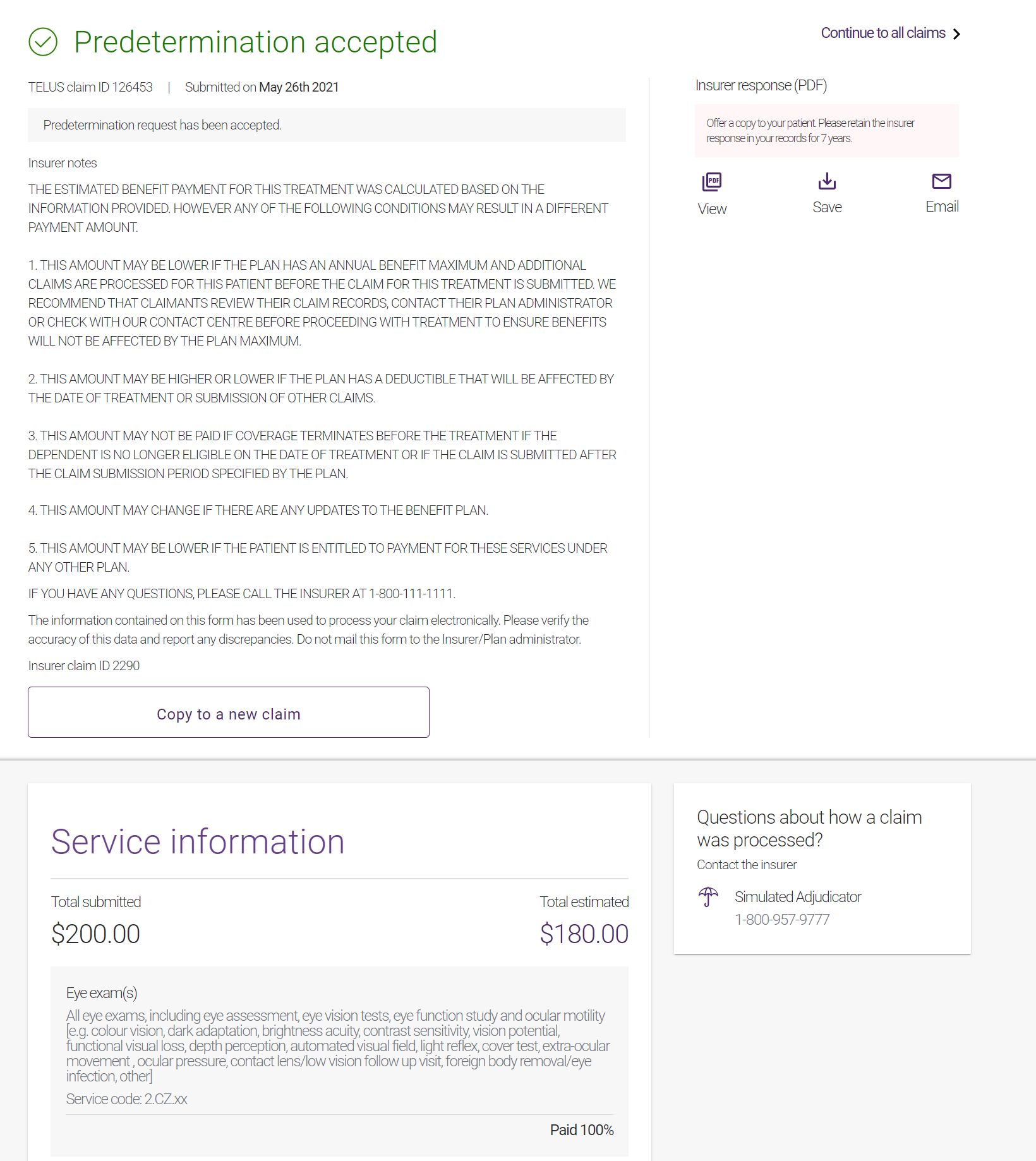
Predetermination accepted
This type of response is generated when the insurance company has accepted the predetermination request. The predetermination response indicates what the insurance company would have paid if the services had taken place on that date.
From the Insurer response (PDF) section, you can view or save the Predetermination Explanation of Benefits, or email it to the patient. The Predetermination Explanation of Benefits response provides the estimated amounts, if any, that would be paid by the insurance company if the claim were submitted on that date.